Is Diabetes an Autoimmune Disease? — All You Need to Know

Diabetes is a common condition that many adults experience globally and is usually considered a major health concern. Currently, there are over 350 million people diagnosed with the condition, while a significant number live with the condition without an appropriate diagnosis. In the United States alone, over 20 million people are considered to have the condition, both diagnosed and undiagnosed.
The stunning increase of diabetes in people has made many health institutions—including the American Diabetes Association (ADA)—carry out various health awareness campaigns on why people should live a very healthy life and eliminate many unhealthy practices that trigger the disease. These campaigns are usually considered from the perspective of diabetes being a metabolic disease that proper health management can prevent. However, new findings over the years have, in a way, suggested that diabetes may not be entirely genetic and metabolic.
Several expert studies and their respective findings suggest there’s a possibility of diabetes being an autoimmune disease. While these studies are continuing, the possibility of diabetes as an autoimmune disease generally affects how people and health experts may consider the condition.
This guide examines what autoimmune diseases are, if the immune system’s natural response may trigger diabetes, and steps people can take to decrease the diabetes risk, including the best diet practices.
What Are Autoimmune Diseases?

Autoimmune diseases are one of the common diseases people develop despite doing nothing wrong. Unlike most conditions triggered by unhealthy choices, extreme stress, and poor exercise, diseases classified as autoimmune conditions naturally occur independently. As far as modern research can show, genetics is the only factor that makes people develop autoimmune diseases.
An autoimmune disease is a major condition where the immune system confuses healthy tissues and cells with harmful invaders, attacking them in the process. The immune system—comprising different immune cells like the T cells and B cells—is scientifically and medically known to fight off diseases that attack the body and do a great job of it. However, there are situations where these cells may malfunction and confuse the healthy tissue that allows the body’s smooth running as invading diseases and attack them.
There are many diseases resulting from immune cells attacking other cells and tissues. Some of these diseases are extremely complicated and are well attributed to causing possible mortality, outlining the risk they project to humans. Some of the popular ones include:
Rheumatoid Arthritis
Rheumatoid arthritis is a condition where the immune system’s B cells and T cells attack the human joints after confusing them with disease-carrying cells. The attack on the joints is often gradual but steady and could cause a range of health discomfort and complications. These include unhealthy warmth in the joint areas of the body, redness, soreness, severe pain, and stiffness in the joint.
Psoriasis/Psoriatic Arthritis
Psoriasis/psoriatic arthritis is another autoimmune disease where skin cells abnormally multiply such that the process of growing and shedding is disorganized due to more extreme supplies of what’s needed. Excessive growth of cells can cause red patches and inflammation, silver-white scales, and joint stiffness.
Blood Cancer
Blood cancer is another condition attributed to the immune cells attacking healthy cells. It’s a possibly fatal condition with a high mortality rate.
Additional Facts on AutoImmune Diseases
From the above, it’s clear that many popular diseases are categorized under autoimmune diseases. We’ve also successfully outlined the danger and health complications these conditions could cause.
Generally, for a disease to be autoimmune triggered, the immune cells must have been evidently proven to attack the human body. Once that’s been established, the disease can be classified to be triggered by autoimmunity.
A key area of focus in this guide is whether diabetes can result from the immune cells attacking human pancreatic islets or any other tissues that directly contribute to insulin production. So, is diabetes an autoimmune disease? This detailed guide successfully answers this question in subsequent sections.
Is Diabetes an Autoimmune Disease? — Breaking It Down
Diabetes is a metabolic disease, implying that it’s a condition that develops following a negative alteration of the body’s metabolism. While there are many classifications of the condition, type 2 diabetes comes to mind following general consideration, possibly due to its widespread nature and impact on general health. Type 2 diabetes has long been considered a problem related to blood sugar levels rise caused by obesity-related insulin resistance and other risk factors.
The second most popular type of diabetes is type 1 diabetes, established as an autoimmune disease. However, since it doesn’t account for most diabetes cases globally, it’s barely regarded as diabetes. Below is a complete definition of the different types of diabetes that people experience:
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition prevalent in children and is characterized by uncontrolled blood sugar rise due to damage to insulin-producing cells. The cell damage is due to the body’s immune cells attacking the healthy cell that supply insulin, making the problem one of autoimmunity.
Type 1 diabetes could be fatal, and children need a constant dose of insulin shots to have their blood sugar under control. As kids grow, though, the condition may faze out. If adequately handled, this phenomenon makes type 1 diabetes more of a temporary problem.
Latent Autoimmune Diabetes in Adults (LADA)
LADA may be said to be the adult version of type 1 diabetes. While it’s not as popular as general type 1 diabetes, it’s not rare among adults. In adults, the immune system cells attack the healthy pancreas cells after mistaking them for disease and infected cells.
LADA is often misdiagnosed and is usually treated as type 2 diabetes — a therapy error since it’s not a metabolic condition.
Type 2 Diabetes
Type 2 diabetes—the more common condition responsible for many serious complications and mortality rates globally—is typically considered a metabolic disease. It’s a condition where our bodies develop insulin resistance due to a poor supply of insulin from the pancreas.
Poor health choices, unhealthy lifestyle activities, and other avoidable factors are the major factors behind developing insulin resistance. So, unlike type 1 diabetes and its related ailment (LADA), people either inherit or develop type 2 diabetes due to risk factors like obesity and high sugar food consumption.
Gestational Diabetes
Gestational diabetes is diabetes that women experience during pregnancy. It’s a temporary condition as women’s blood sugar levels usually return to normal after childbirth. It’s one of the recognized type 2 diabetes, and women who experience it are at a higher risk of developing type 2 diabetes later if they don’t implement healthy practices.
So, Is Diabetes an Autoimmune Condition?
From the above points, it’s clear that type 1 diabetes is an autoimmune condition, while type 2 diabetes is considered a purely metabolic disease. However, type 1 diabetes and its subgroup, LADA, are mostly temporary and significantly rare. On the other hand, type 2 diabetes and its related condition, gestational diabetes, are common. Type 2 diabetes, in particular, could be—and is usually—a permanent feature in the lives of many people diagnosed with it.
Diabetes experts have only considered type 2 diabetes from the lens of it being a metabolic condition. It’s believed to occur when people’s life activities affect their health such that their cells promote insulin resistance.
However, new studies prove that type 2 diabetes may not be a 100% metabolic condition. In fact, there have been some convincing research that places it as a condition triggered by adaptive immune responses. While type 2 diabetes being an autoimmune condition hasn’t been fully confirmed yet, if acknowledged as such, it becomes similar to type 1 diabetes and alters its treatment options.
What the Experts Say: A New Outlook?

Although there are considerations that push the ideology of diabetes being an autoimmune disease, health institutions haven’t formally confirmed this line of thought. However, this doesn’t imply that the condition isn’t connected to improper functioning of the immune system targeting diabetes-preventing cells.
Several studies indicate that type 2 diabetes could be an autoimmune condition just like type 1 diabetes, as pathogenic IgG antibodies were used to treat some of the immune cells that are believed to play a major role in triggering diabetes. The majority of these studies on type 2 diabetes showed that while other factors cause the condition, the possibility of the immune system targeting other healthy cells and tissues is also an eligible factor.
The Nature Medicine journal published one of the most reputable studies on diabetes being an autoimmune disease. The institution focused its research on finding treatments for type 2 diabetes by targeting the immune system instead of the traditional move of controlling blood sugar.
The study suggested that the B cells, a major part of the immune system, are among the causes of type 2 diabetes. The researchers who performed the study on mice used the anti-CD20 antibody to eliminate mature B cells in some samples, and the result showed that those with lesser B cells were less prone to the progression of type 2 diabetes.
The result was remarkable as anti-CD20 is a popular antibody for treating chronic advanced autoimmune diseases, including blood cancers. For the mice that didn’t get anti-CD20, the mature B cells and other related cells in the immune system attacked healthy tissues, including the cells that produce insulin. This particular trend drew an overlapping situation between type 1 and type 2 diabetes as the former is also triggered by immune cells attacking insulin-producing cells in children.
Daniel Winer, an endocrine pathologist and major scientist in the study, remarked that the study had the potential to redefine what’s known about type 2 diabetes and the reality that it may not be solely a metabolic disease. He further stated that confirmation of the condition as autoimmune-related will also impact medicines and treatments used for controlling the condition. Notably, alterations will have to be made so that drugs and other management tips focus on reducing the impact of immune cells on the disease.
The study, “Type 2 Diabetes: How Much of an Autoimmune Disease”, outlined the possibility of type 2 diabetes being considered autoimmune diabetes. The study didn’t consider any respondent for data but rather the progression of diabetes and its connection to other important cells like the B cells.
The research identified why ageing and obesity are the major causes of type 2 diabetes progressing into reality and causing further complications. There’s a possible connection between the disease and a low-grade inflammation triggered by the immune system attacking healthy cells and tissues.
The research—which cites other publications on diabetes as an autoimmune condition—states that evidence points to low-grade inflammations causing insulin resistance (IR) and beta-cell failure, a common feature in type 2 diabetes. Inflammation also causes the body to have an increased demand for insulin that can’t be met while triggering the development and destabilization of atherosclerotic plaque.
Apart from the inflammation autoimmune disease causes, the study on people with type 2 diabetes also pinpointed other psychological distress common in people with autoimmunity. It revealed lack of self-tolerance to be common in people with type 2 diabetes due to chronic and excess B cells and T cells reactivity.
The two studies highlighted are among the few that successfully suggest type 2 diabetes to be an autoimmune condition. On the one hand, the second study confirmed that inflammation triggered by the immune system does cause slow but steady progress of the disease in people. On the other hand, Winer—the major scientist in the first study—confirmed in another study that lifestyle factors cause the reaction of the immune cells.



According to Winer, in an independent study, mice exposed to significantly high-calorie foods had more risk of the B cells attacking the insulin-producing cells.
How Does the Possible New Implication Affect Current Day Treatment?

Generally, type 2 diabetes has been considered a metabolic condition that could degenerate into worse complications like fatty liver disease caused by too many fatty acids, heart disease, kidney failure, and stroke. However, considering what research now shows, it’s possibly more than that and could also result from autoimmunity.
The studies show that type 2 diabetes could develop from low-grade chronic inflammation following an attack on immune systems cells. This new revelation means that diabetes treatments may need to undergo significant changes to handle the new type 2 diabetes better. It’s believed that these changes could finally help treatment focus on type 2 diabetes control more effectively.
Currently, the two major ways doctors treat diabetes are through lifestyle adjustments and medications. The former comprises healthy living, dieting, and keeping fit — a strategy whose overall goal is to achieve consistent blood sugar control and weight management. Since obesity is linked with the condition, doctors usually recommend lifestyle adjustments as the healthiest and most natural way to tackle diabetes and blood sugar.
The other form of controlling type 2 diabetes is through medication. Some of the more common treatments are GLP-1 RAs and insulin injection. These medications are targeted to decrease blood sugar levels and improve insulin sensitivity.
However, since there’s now the possibility that type 2 diabetes is also an autoimmune condition, the new treatment expected to be included for its management would be immunosuppressant medications.
From the expert studies considered, it’s obvious that one of the treatments that doctors will bank on is the anti-CD20 antibodies. The main medicine packing these antibodies is Rituximab which has been proven to successfully reduce the immune cells (B cells and T cells) that attack the pancreas and other insulin-producing cells.
While anti-CD20 is currently effective for handling almost all types of autoimmune disease, the progress achieved in the mice experiment—where it eliminated the mature B cells that attack the insulin-producing cells—makes it a viable option to look up to. Over time, health experts are also expected to develop more immune suppressants to treat the condition.
Examining Other Diabetes Risk Factors
Diabetes is likely to be declared an autoimmune-metabolic disease in the future. However, it’s still considered a metabolic disease due to the extremely high connection with many lifestyle factors.
As such, it’s critical that people at risk of the condition or having the ailment take already established health practices seriously. To achieve this, there’s a need to apprise oneself of other risk factors that contribute to its development and further life-threatening complications.
Below are the risk factors that people with diabetes should be aware of.
Age-Related Factors
Diabetes is most likely to affect people as they age. The American Diabetes Association (ADA) reports that 25% of people with diabetes in America are 65 years and above. Moreover, the Center for Disease Control and Prevention (CDC) recommends that adults over 45 years should get tested for diabetes. This indicates that older adults and middle-aged people are at a high risk of developing diabetes.
In 2015, people in the 45–64 years age group accounted for a large proportion of those diagnosed with the disease. Here’s a clearer outline of the distribution:
- 355,000 people diagnosed with diabetes were from the ages of 18 to 44
- 366,000 people diagnosed with diabetes were between the ages of 65 and above
- 809,000 people diagnosed with diabetes were between the ages of 45 to 64
Medical Conditions
People who have the following medical conditions are at a high risk of having diabetes:
- Hypertension higher than 130/8 mmHg
- Polycystic ovary syndrome
- High levels of cholesterol
- 250 mg/dL or higher levels of triglyceride
- Acanthosis nigricans: A skin condition that causes the skin to look darker than normal
- High blood sugar that’s not normal or pre-diabetes
- Gestational diabetes in women that give birth to babies weight 9 lb or more (increased type 2 diabetes risk)
Environmental Factors
Individuals who had an unknown virus at the early stage of their life could develop type 1 diabetes. Other people living in cold climates are also likely to have the disease. This is why doctors diagnose more people with diabetes in the winter than in the summer. Research also shows that air pollution could put you at a higher risk of having diabetes.
Genetic Factors
Doctors haven’t found the root of type 1 diabetes. People who have a family member with type 1 diabetes have a high risk of having the condition. According to the American Diabetes Association (ADA), anyone who falls under the following category has a chance of developing type 1 diabetes:
- A person whose father has type 1 diabetes has 1 in 17 possibilities of having the condition.
- A person whose mother has type 1 diabetes has 1 in 25 possibilities of having the condition if born when their mother was younger than 25. If the woman had the child when she was 25 years or more, the child has 1 in 100 possibilities of having type 1 diabetes.
- A person whose both parents have type 1 diabetes has between 1 in 4 and 1 in 10 possibilities of having the condition.
Additionally, a parent with type 2 diabetes also exposes his offspring to the risk of having the disease. This is because diabetes is connected to lifestyle. Children can inherit poor habits from their parents and a genetic predisposition.
All of these factors either increase a person’s risk of having either type 1 or type 2 diabetes. However, people from certain ethnic groups are also at risk of developing type 2 diabetes. The following ethnic groups put people at risk of having the disease:
- Native Americans
- Pacific islanders
- Asian Americans
- Hispanic Americans
- African Americans
Additionally, women who have a family member with gestational diabetes have a higher risk of having the condition.
Lifestyle Factors
It’s still unclear if lifestyle factors increase one’s risk for having type 1 diabetes. However, lifestyle choices determine a person’s risk for type 2 diabetes. These are the lifestyle factors that put people at risk for the disease:
- Physical inactivity
- Unhealthy diet
- Smoking
- Obesity
The American Academy of Family Physicians (AAFP) regards obesity as the highest risk factor for developing type 2 diabetes.
How to Prevent Diabetes
In the above section, we considered some of the major risk factors that cause type 2 diabetes. Currently, the established diabetes risk factors are the only major cause of the condition since its autoimmunity hasn’t been globally recognized.
Here, we outline some of the natural means that people can use to control high blood sugar, live more healthily and prevent the risk of autoimmunity as much as possible.
Eat Food High in Fiber
Eating food with fiber is essential for weight management and gut health. It could also prevent or reduce your risk of diabetes. Research on prediabetic people and old women with weight issues suggests that fiber helps lower insulin and blood sugar levels.
Fiber can be grouped into categories of soluble and insoluble. Soluble fiber absorbs water while insoluble doesn’t. Water and insoluble fiber create a gel in the digestive tract that causes a decline in food absorption resulting in a slow rise in your blood sugar. So, eating foods with soluble fiber can reduce insulin and fasting blood sugar levels.
Research has also linked insoluble fiber to lowering blood sugar. Many studies on diabetes and fiber focused on supplements, but foods high in fiber are likely to be more beneficial in preventing diabetes.
Cut Down Consumption of Processed Foods
Reducing the intake of processed food will benefit your health in general. While many foods go through processing, processed foods containing frozen vegetables and plain yogurt aren’t naturally unhealthy. Thus, highly processed foods contain chemical preservatives, added sugar, and unhealthy fats.
Examples of such food are chips, soda, hot dogs, candy bars, and frozen desserts. An observational study links a diet high in processed food with the risk of type 2 diabetes.
Similarly, cutting down processed foods high in additives, refined grain, and vegetable oil could help lower your risk of diabetes. This is because of the anti-diabetes impact of whole foods like fruits, nuts, and vegetables. Remarkably, research shows that a diet with highly processed food increases your risk for diabetes by 70%, while eating whole foods lowers such risk.
Stay Active
It’s essential to stay active and reduce sedentary behaviors like sitting all through the day or getting little physical activity to help prevent you from having diabetes. Observational research has consistently connected sedentary behaviors with a high risk of type 2 diabetes. A study of over 6,000 elderly women discovered that those who indulge in sedentary behaviors for 10 hours or more in a day had an increased risk of diabetes than those who had eight hours or less of inactivity.
Staying active could involve spending a few minutes walking around every half hour or walking a short distance instead of driving. You can use a fitness device or watch to help remind you to take a walk every hour.
However, it can be challenging to cut back on entrenched habits. Research that designed a one-year program to help young adults at risk of having diabetes stop their sedentary behavior discovered that they did not reduce their sitting time. Hence, it’ll be best to set realistic goals like taking the stairs when you get the chance or standing while on the bus even when there are free seats.
Avoid Salt if You Can
Cut down on the salt in your meals as it could help keep your kidney safe and reduce your blood pressure. It may not be enough to stop adding salt to your dish before eating. This is because most of the salt in our diet is found in processed foods.
So, avoid processed food and use fresh ingredients for cooking if possible. When cooking, choose spices and herbs over salt. It’ll be best to talk with your doctor about the amount of sodium ideal for you daily.
Summing It Up
This comprehensive guide has successfully considered the possibility of diabetes being an autoimmune disease. While type 1 diabetes is undoubtedly an autoimmune disease, the more popular type 2 diabetes—known for causing the majority of diabetes corporations and death—has been treated as a metabolic disease for decades. However, new studies discussed in this guide suggest there may be some connection between diabetes type 2 development and immune cell attacks.
However, it’s important to know that there’s no major confirmation of type 2 diabetes being an autoimmune disease. While it does have the characteristics common with normal autoimmune disease development, more research is needed to confirm that it’s indeed an autoimmune condition. Since the condition is yet to be acknowledged fully as autoimmune-related, it’s best treated with traditional and lifestyle practices.
Although there are many lifestyle choices one can take to better their diabetes condition, eating the right meal trumps all of them. As outlined in this piece, eating healthy, diabetes-friendly foods can help you control the progression of type 2 diabetes and even effectively reverse the condition. More importantly, food choices control your health and even determine to what extent exercising can work in controlling your condition.
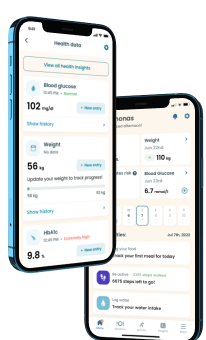
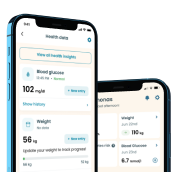
There are several ways you can always eat diabetes-friendly meals. First, you can seek the help of a dietitian or an endocrinologist for expert recommendations on the best food to eat. Alternatively, you could use a diabetes meal app with expert diabetes meal app recommendations.
Our diabetes management app, is one of the quality resources people with the condition can trust to help them make excellent decisions regarding their food choices. The icing on the cake is that our team of experts regularly updates this virtual caregiver with the newest changes so patients can select the best meals for them in terms of taste and health.
Take a quiz and get your diabetes-management plan today!